Nutrients & Diet for Eye Health
At some point in all our lives we’ll hear our doctor say, “You know, you really should be taking a daily multivitamin.” The simple fact is that as people age, they tend to reduce their overall consumption and absorption of necessary vitamins and minerals. In fact, fifty percent of older adults have a vitamin and mineral intake less than the recommended daily intake (RDI), while 10%–30% have subnormal levels of vitamins and minerals¹.
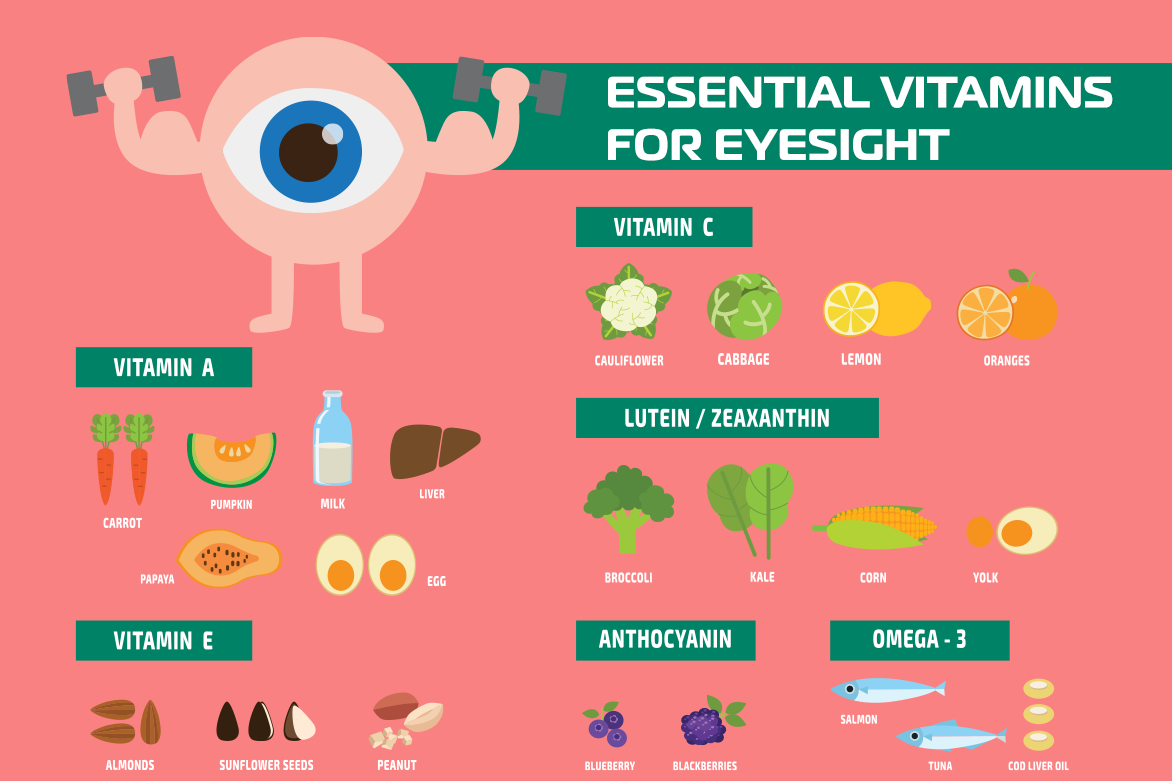
Besides well-known nutrients like vitamin C, calcium, iron, magnesium, and potassium, a standard multivitamin will also include thiamin, riboflavin, niacin, vitamins B6 and B12, folate, selenium, and zinc.
Eye Health Research
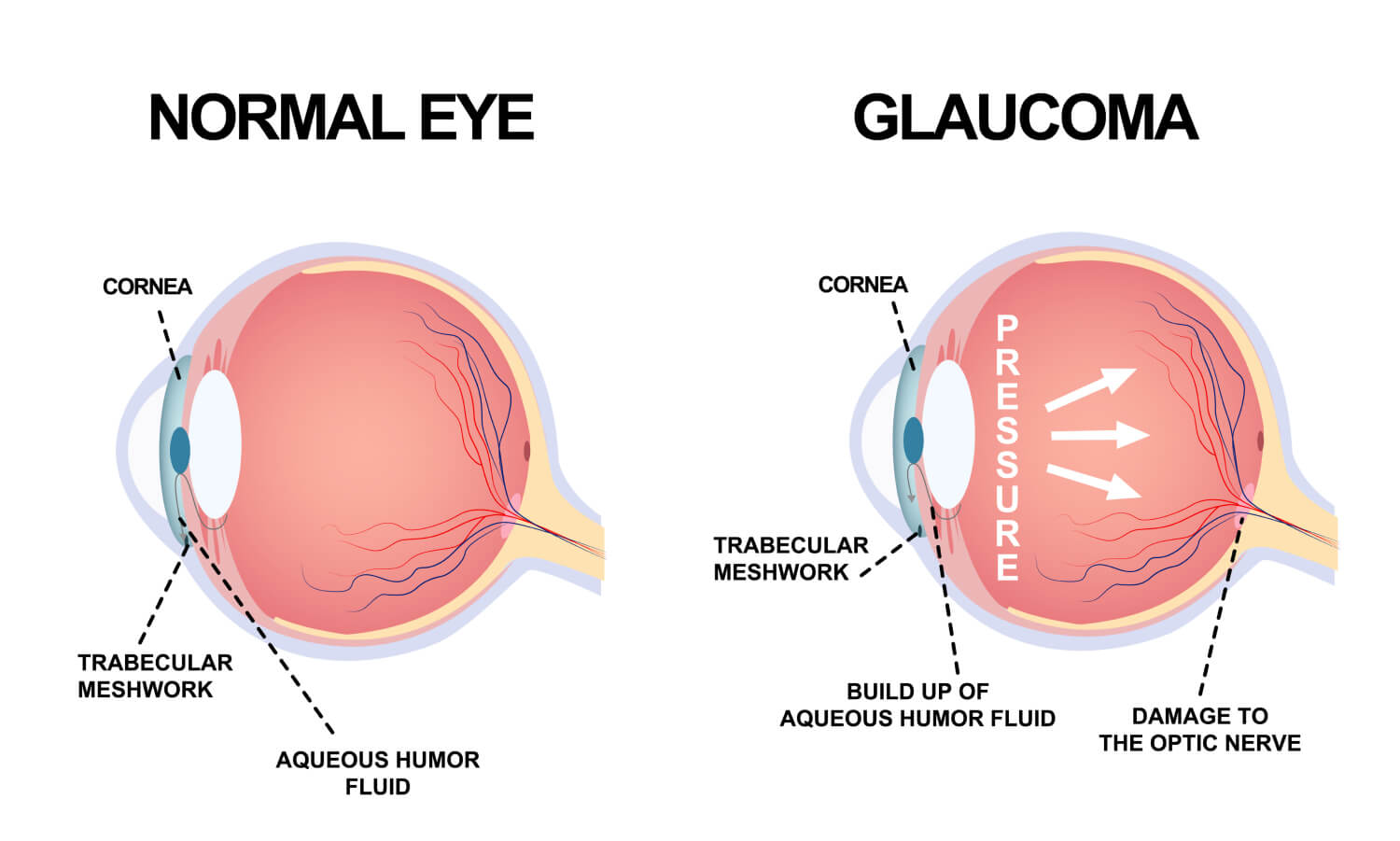
In 2001, the National Institute of Health launched the Age-Related Eye Disease Study (AREDS), a major clinical trial designed to learn more about the causes and risk factors of age-related macular degeneration (AMD) and cataracts and to evaluate the effect of certain vitamins and minerals on those disease factors.
This study specifically looked at vitamin C, vitamin E, beta-carotene, and zinc. Results from the study showed that high levels of antioxidants and zinc significantly reduced the risk of advanced AMD and vision loss associated with the disease while showing no significant effect on the development or progression of cataracts.
Eye Health Supplements
Researchers with the AREDS study took their findings and created a nutritional supplement called the AREDS Formulation, designed specifically to reduce the risk of developing advanced age-related macular degeneration. The original formulation contains vitamin C, vitamin E, beta-carotene, zinc, and copper. Vitamins and minerals the study deemed vital and important to overall eye health. Both AREDS and AREDS 2 formulations can be found in various supplements at your local pharmacy.
The broader vitamin and supplement market has also been jumping on the eye health bandwagon including a supplement called Ocuvite from Bausch + Lomb is marketed to “Help Protect Your Eye Health” with ingredients including Vitamins C, E, and D, as well as zinc, copper, Omega-3 fatty acids, Lutein and Zeaxanthin, both marigold flower extracts – two carotenoid nutrients, a type of antioxidant, found in the eye that help strengthen the macula, the part of the eye responsible for shielding and filtering high-energy blue light.
There are countless other supplements on the market for eye health as well all delivering those same essential vitamins and minerals for both overall physical health, mental acuity, and eye health.
The Best Protection For Your Eyes
Far and away the best thing you can do for the health and wellbeing of your eyes is to get annual eye exams at your eye doctor. Protect your eyes from ultraviolet light, get plenty of sleep, eat well for eye health, and again, make sure you see your eye doctor once a year for an annual exam – it’s the best vitamin you can take!
Read More