Glaucoma Treatment
If you’ve been diagnosed with glaucoma, you’re probably already familiar with the typical options in glaucoma treatment – eye drops, laser treatment or traditional surgery. While these are certainly effective, especially when glaucoma is diagnosed early, researchers have been working hard to offer new glaucoma treatments. Their goal is not only to improve outcomes but also reduce the treatment’s side effects and frequency of use.
What Is The Goal Of Glaucoma Treatment?
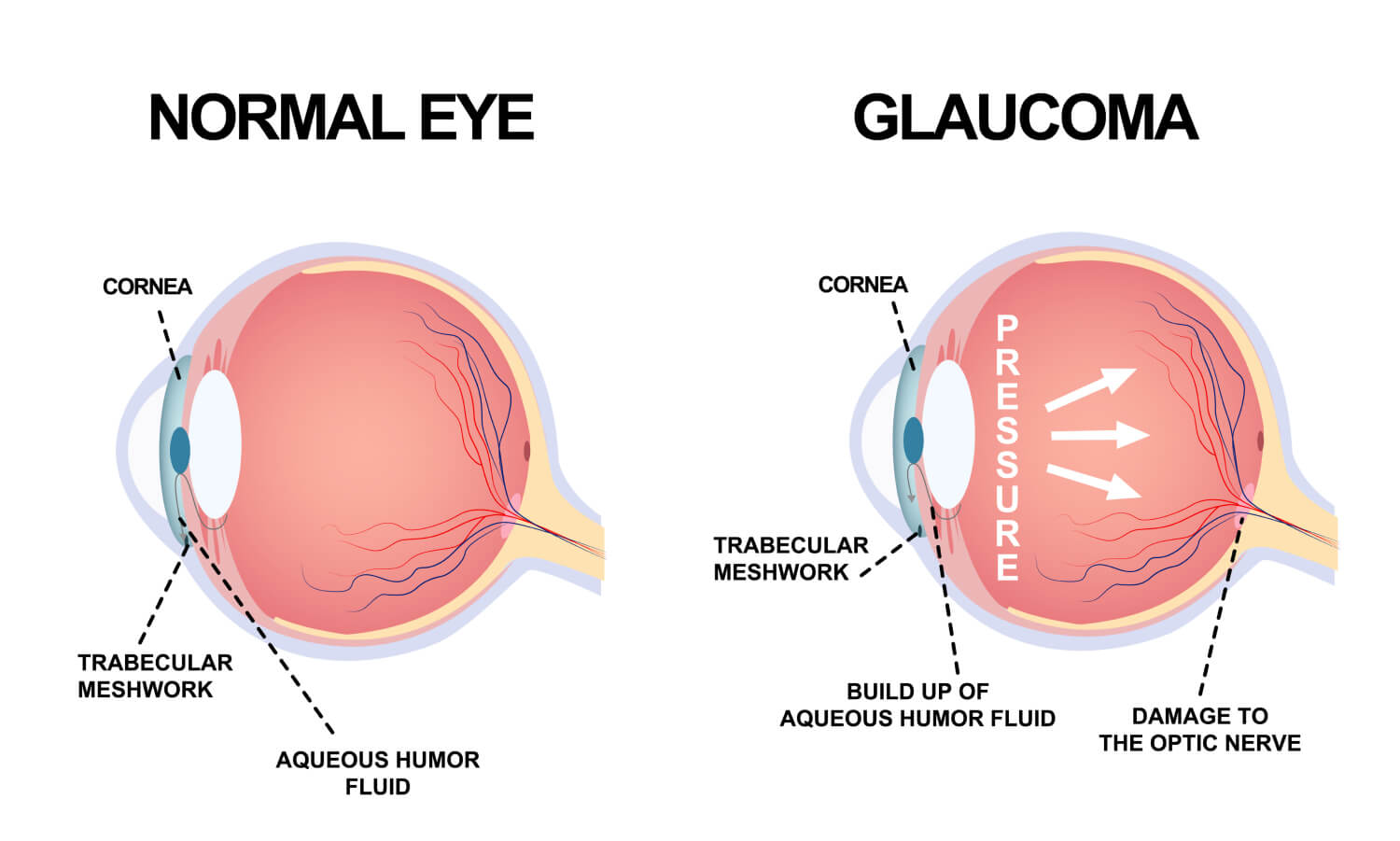
Before we dive into the new options, it’s important to understand the goal of any glaucoma treatment. At present, glaucoma is not curable. However, treatment can significantly slow the progression of the disease. Glaucoma damages your eye’s optic nerve. Extra fluid builds up in the front part of your eye (cornea), which increases the pressure in your eye. Reducing this pressure is the primary objective of any glaucoma treatment. This is often referred to as intraocular pressure or IOP.
What Are The Limitations Of Standard Glaucoma Treatments?
Eye drops for glaucoma treatment seem like an easy option but there are several challenges that can reduce its effectiveness. It can be difficult to get all the medicine in the eye, especially for older adults with less of a steady hand. In addition, since it must be applied daily, individuals may forget. Since the drops have no perceivable benefit because early stages of glaucoma have no symptoms, patients might make it a lower priority which is understandable since it may also have unpleasant side effects like burning, red eyes.
Beyond eye drops, laser surgery is a less invasive option. The laser opens clogged tubes and drains fluid. It can take a few weeks to see the full results. If laser surgery or drugs don’t relieve your eye pressure, you may need a more traditional operation. You would have to go into the hospital and will need a few weeks to heal and recover. Although usually effective, glaucoma surgery can make you more likely to get cataracts later on. It can also cause eye pain or redness, infection, inflammation, or bleeding in your eye.
What Are Recent Advances In Glaucoma Treatment?
Alternatives or Improvements to Eye Drops
The Glaucoma Research Foundation reported several new developments on the horizon. These technologies focus on reducing patient error in applying eye drops which would make the medication more effective and improve the quality of life for the patient. Here are some of the products underway:
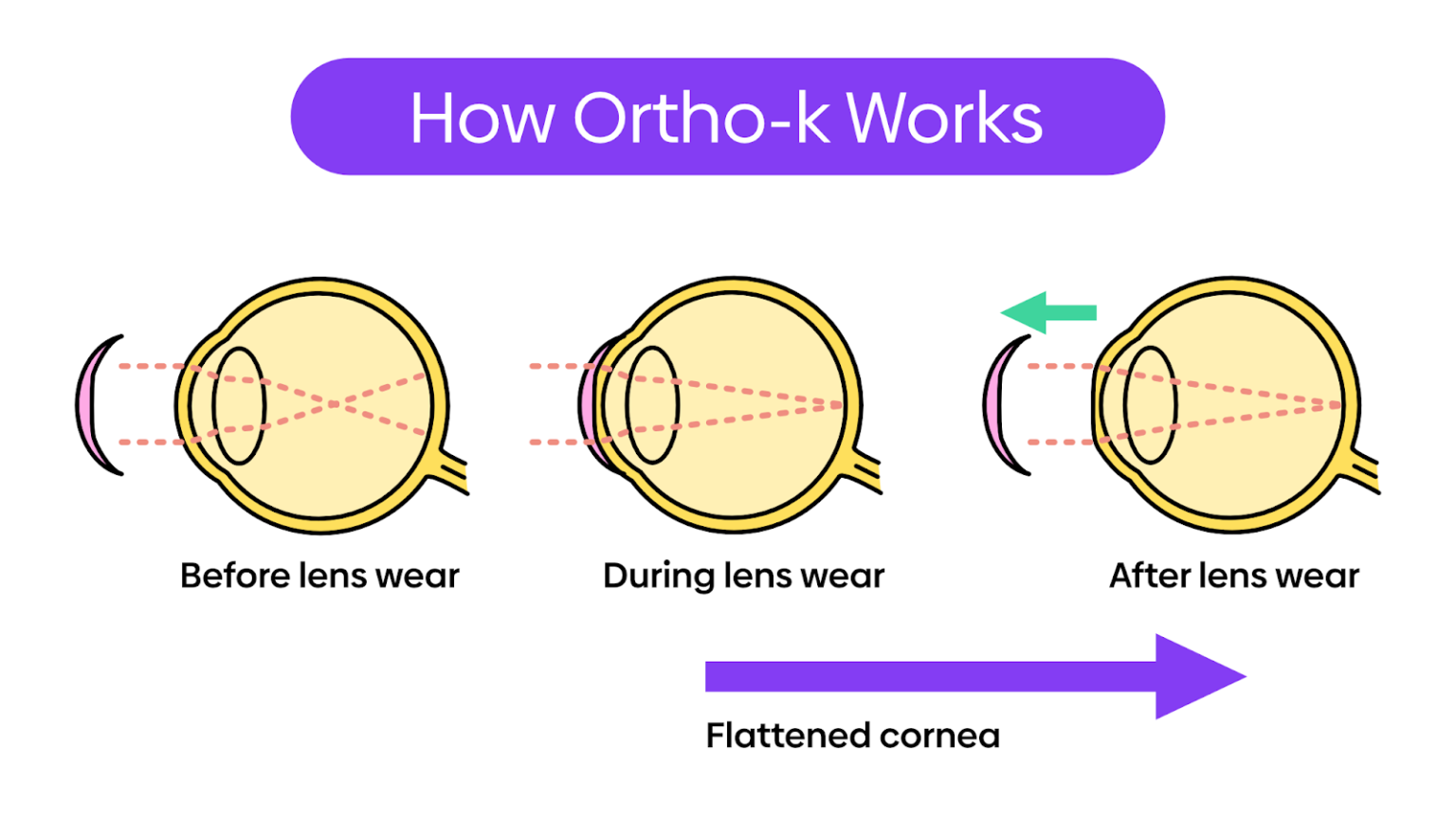
- A polymer, like a contact lens, would contain the drug; it would sit under the eyelid and release the medication over several months
- Microneedles would inject medication into a specific spot to be most effective
- Implantable extended-release devices using engineered highly precise microparticles and nanoparticles
- Polymer-based intraocular delivery technologies that would allow customizable sustained release
- Drops that allow the medication to get into the eye more easily
- Tear duct plugs that release medication
In addition, people with glaucoma who take more than one eye drop per day are beginning to see those medications available as a single, combined eye drop. New products include Cosopt (timolol and dorzolamide), Combigan (timolol and brimonidine) and Simbrinza (brinzolamide and brimonidine).
Minimally Invasive Glaucoma Surgery
Minimally Invasive Glaucoma Surgery (MIGS) procedures are small cuts or micro-incisions through the cornea that cause the least amount of trauma to the surrounding tissues. Doctors implant a tiny device to allow fluid to drain from the eye, reducing internal pressure. Some devices (iStent) are implanted during cataract surgery. Cataract surgery alone lowers pressure, but the combination of both is more effective and can lower the need for medication.
These new techniques minimize tissue scarring, allowing for the possibility of traditional glaucoma surgery in the future if needed. They also give doctors the opportunity to treat patients earlier and more safely than older surgeries.
Monitoring Eye Pressure
An easy, accurate way to measure eye pressure is critical to monitoring the progress of glaucoma and adjusting treatment as needed. For patients that require more frequent testing of their eye pressure, there’s now an at-home tonometer called iCare HOME. There’s no puff of air and no eye drops. The patient can easily share the information with their eye doctor.
If you have a glaucoma diagnosis, you can feel confident that your glaucoma treatment options are only going to improve in the years ahead. Although the disease is not curable, it is very manageable with the right treatment.
Read More